I wrote this post last fall -- and left it to 'simmer' under my drafts, until I felt I could more fully, and more maturely, develop it.

It's cool outside. The air is crisp, and clean; tinged with so much moisture that I can feel its mist on my cheeks. Wondering home after work, in the early afternoon, gives me pause. The crunching leaves underneath my feet, the neon yellow colors, and the scent of trampled ginkgo biloba wakes me right up. Ginkgo biloba is pungent, that's for sure; it's scent is something between icky bodily functions, and rotting flesh.
No matter though. The heavy atmosphere begins to release a mild rain... and though there's no umbrella and it's quite cool outside, I find myself embracing the very awareness of being alive that the new season brings upon my senses.
I realize, suddenly, that I love Fall. But then, don't I also hate it sometimes? I know I've told myself that before... Why is that?
[Walking gives one much time for thought. Deep thoughts by Jack Handy kind of thoughts, I guess. (If you hate walking for the exercise, well, at least love it for the thinking.)]So... what is it that I love about Fall, or any season, anyway? The answer is both obvious, and not so obvious; one of those much clichéd "Aha!" Oprah kind of moments. I love seasons because of their promise of
RELIEF.
This brief moment of relief brings my soul much healing from the previous season; a much needed break from the burden of dealing with whatever else was before. Yes, relief. You see, I start out loving a season, and then it slowly becomes annoying to me, and outright burdensome... I then get sick of it, or even depressed from it. I get sick and tired of the stupid season! It seems long, and never ending... and there's only so much of -20°F or 100°F (and everything in between) one can tolerate. So, every new season brings me relief from the
previous season. It brings me a much welcome change of pace
. It brings me an opportunity to love life again. To smile... to take in the wonder of how much nature can change from one moment, to the next.
And it's much the same with diabetes, and our "seasons" of self care, isn't it? We make up our minds to begin caring for ourselves, anew, and start out with the joyful promise of good things to come... and then we get sick of it. We seem to perpetually live in one season, and one season only -- often with little flexibility with our routines; we impose the new "season" on ourselves --with strong militance -- and then we burn out. Then after a little while, we start yet another season, but with the mindset of 'rectifying the previous bad behaviors.'
But, should we change things before our "season" changes
us into something we don't want? Maybe we ought to begin a new season simply pondering what lead to the 'bad behaviors' in the first place... I know I'm guilty of it, particularly with my routines. With it's dietary calculations, carbohydrate juggling, testing, supplements, medication management, exercise routines, and doctors appointments -- diabetes can be one long, and boring, and often, depressing season. Some people thrive in that kind of season, just like some love perpetual sunny days... but once in a while, my soul needs a little rain.
So, how do we avoid this cycle? What can we do so that we don't get stuck being miserable, in a crappy season, and completely giving up on diabetes management, over and over again? Well, it's obvious that we're creatures of spontaneity -- we need, and crave change, so wherever we can, we must allow ourselves some flexibility. With this in mind, we must take a moment to consider...
a.) Which things are negotiable; and
b.) Which things are not negotiable.
And we must be realistic. We need to sit down with ourselves, and realize that we simply cannot put everything in the "not negotiable" camp. For example -- as much as I, in principle, would love to eat nothing but eggs, every morning, so that I have the best blood glucose numbers -- I know that I am quite sick of eggs. I don't want eggs all the time; I don't want flax seed meal muffins, I don't want weird food. I want to eat a chicken soft taco, with lots pico de gallo, lettuce, and a little hot sauce. It's about 35-40 carbs. IT'S FINE. My morning blood sugars aren't below 100, but quite frankly, they don't go over 150, either... and I'm okay with that.
Will I have a bunch of cereal, of any kind, for breakfast? No. Cereal is not negotiable for me, and not even because of the spike. It's just not satisfying to me -- psychologically, it doesn't seem like I've eaten anything, and physically, it just doesn't fill me up. It makes me need more food, and I'm not much of a pleasant morning person to be going around, making extra things. I tend to like regular meals at that hour, OR, a light snack and a brunch later on. If we think about it, most breakfast foods are just an excuse to eat desserts in the morning, anyway. So... I'm not going to kill myself with eggs, nor cereals, nor weird substitutes.
Now, in my desire to eat with awareness, what I seek to avoid is binging; that is not negotiable. (As non-negotiable as completely giving up testing.) Overeating may happen from time to time, as we learn our limits -- but binging is not negotiable. So, what does my body want to eat, intuitively, the most? These days, my body wants and craves veggies the most. Non-starchy veggies, and lean proteins. Sometimes, though, I might crave a bit of creamy tomato soup, with a small portion of gnocchi in that soup -- and I can have that. I need to recognize, though, that I will NOT and CANNOT live forever on just veggies, and just protein. That the occasional starch and/or grain is okay -- even if it's not 'whole.' I am perfectly aware that this is not deadly, that it is not untenable, and that some people make the change, without issue -- but if I did this, I know I would soon fail. I am not a person, psychologically, to endure such a restriction -- to endure deprivation and strict eating rules. I do eat low carb most every day -- but every once in a while, I am OKAY with my blood sugar not being perfectly below 120 after every meal. If it's below 160, sometimes, it'll do. Yes -- it'll do. So... I tend to cycle some days when I eat very low carb, with some when I eat moderately low carb, and with some when I allow myself a treat.
Studies have shown that an intermittent low carb diet is still much better at reducing insulin levels in one's blood, than a Mediterranean diet (or standard dieting). We're not speaking of insane changes, here... It's not like I'm going to sit out in the rain all day, because I got tired of sunny days. (No, no... sorry, there's not going to be an "all brownie day." Put down the icing.) But maybe one or two days of splashing in some puddles might do me some good. After all, who wants to go to a favorite restaurant and ALWAYS have to stick to the same food option?
No one. They'd soon fail. So then, we must learn to be realistic, and keep a balance between our own desires for freedom, spontaneity and change -- and our limitations.

Another change in season which we may consider, is simply changing how we view the way a meal affects us. Not every meal is going to be perfectly within blood glucose goals -- but perhaps the bigger question should be: "how well do I feel when I eat it?" Quite frankly, I have to limit heavy breakfasts -- proteins with too much fat, or calories, will make me feel bogged down and sick -- even if they give me great numbers. Most of the time, I cannot handle a great work day, if I'm bogged down in a very heavy breakfast. I also can't eat very bitter or tart foods at that hour, like yogurt, or grapefruit. Hey, I admire the people who eat that every day, and can get away with it -- but it seems to be unsatisfying to me, both physically, and emotionally. On the other hand, a home made tomato soup, with lots of veggies, and a bit of gnocchi -- while giving me blood glucose levels sometimes in the 160s -- make me happy, joyful, and healthy. And the highs do not last very long. Since I've started eating more like this, I've also had better fasting numbers in the mornings -- usually in the 80s.
But perhaps, by far -- one of the things we ought to consider when managing our 'seasons' with diabetes, is to enlist the help of our friends and family. If one has a "Type 3" person enlisted in one's care, one should use this moment now to plan out a 'new season' with them. That could be as simple as choosing one or two weekends a month, where
they are the person who makes meals, so that you don't have to be the main meal maker ALL the time. Or, it could be the other way around... maybe
we can be the main meal maker, so that we give one's Type 3 a break from having to make
our meals all the time. Learning to plan, and prepare, diabetes-healthy meals can be a lot of fun, sometimes.

What concessions are we willing to give ourselves in order to learn why the caged bird sings? Diabetes is a steady stream of seasons; it's best to let ourselves change and flow with the wisdom they bring. I'm only 36, and I have a good 30+ more years with this disease, so I have to learn to run a good race... and be consistent at it. This, for someone like me, is a HUGE challenge... and though I may seem like I have it all together, believe me, I'm still, very much, a work in progress.
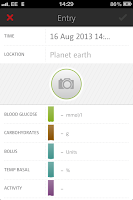
I never have quite the same consistent answers about my eating habits, or exercise routine... because well, there is no consistent answer. I simply try to do whatever makes me feel healthy, so long as Mr. Meter approves... and I'm not sick of it. Mr. Meter, though, is going to have to learn to be a bit more flexible, sometimes. Or he'll end up decorating my wall. As you can see by this 14 day average, he can be a real drill Sargent, sometimes... even with those silly, googly eyes.
In order to survive, we need to change our seasons. We need to redecorate, to transform, to change the same four 'diabetes walls' we stare at, every day... because we need
RELIEF.
Sometimes, our souls just need a little rain.